Edited by Admin_Dermpath
Case Number : Case 1870 - 28 July - Dr Richard Carr Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
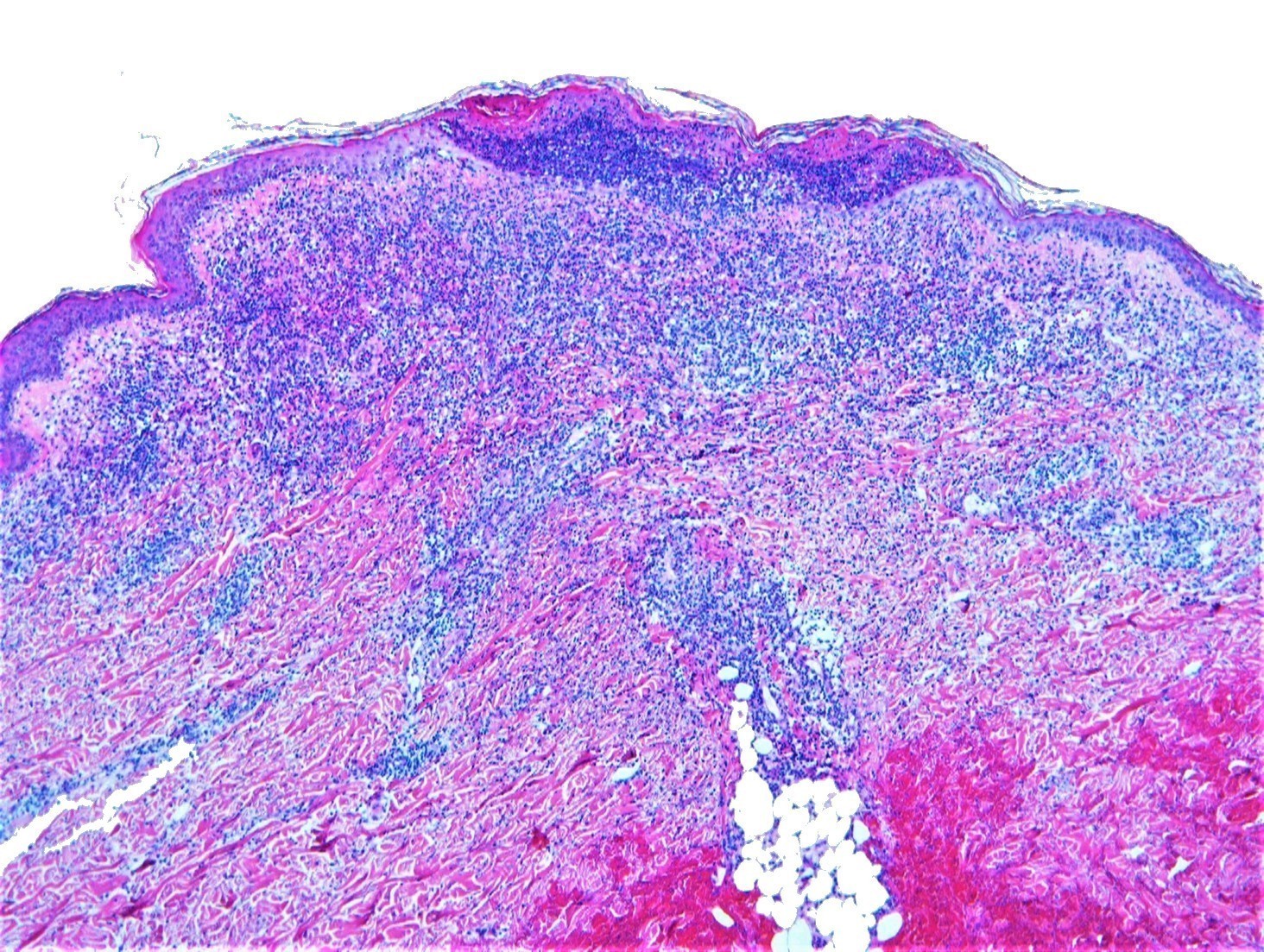
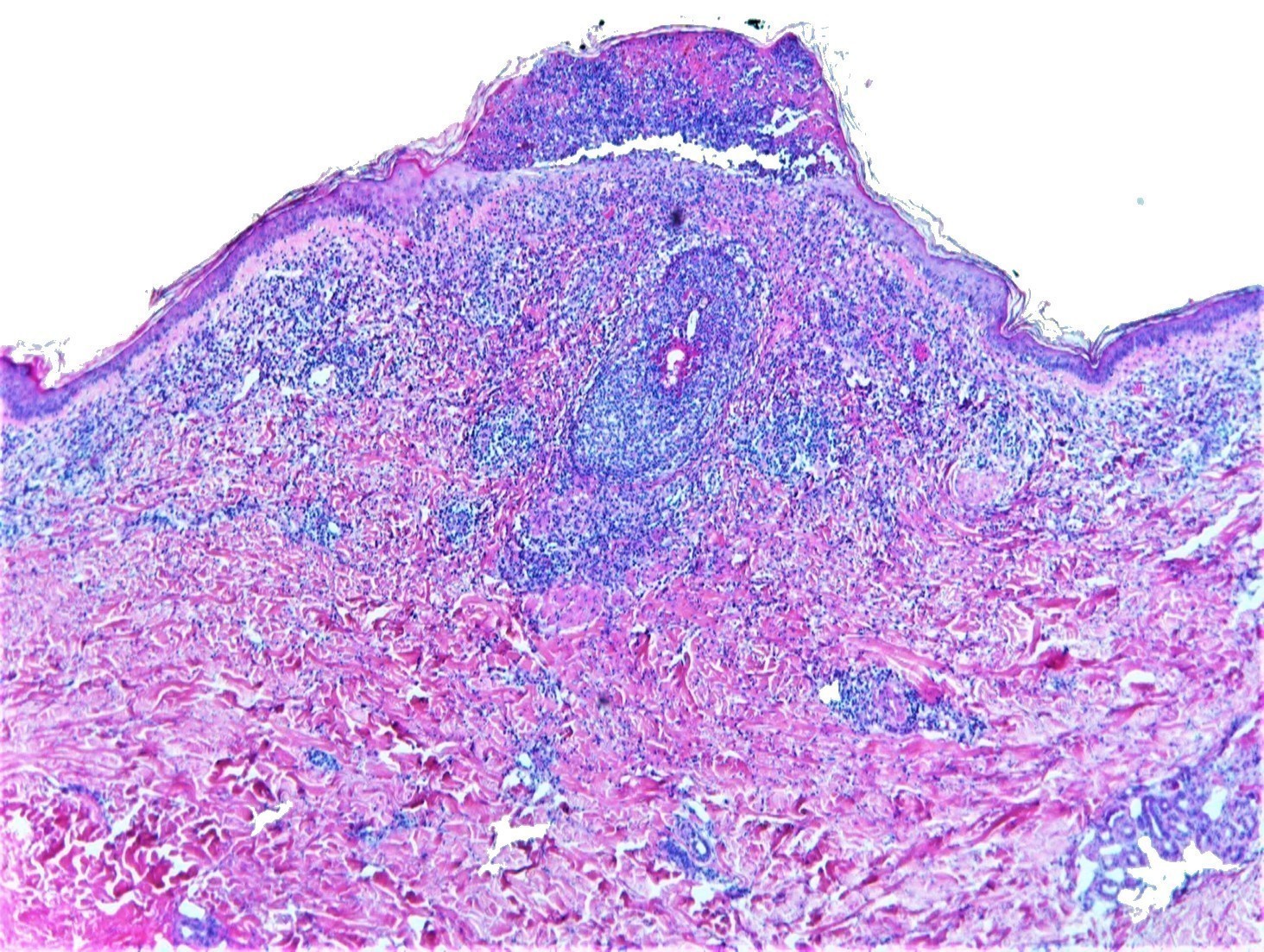
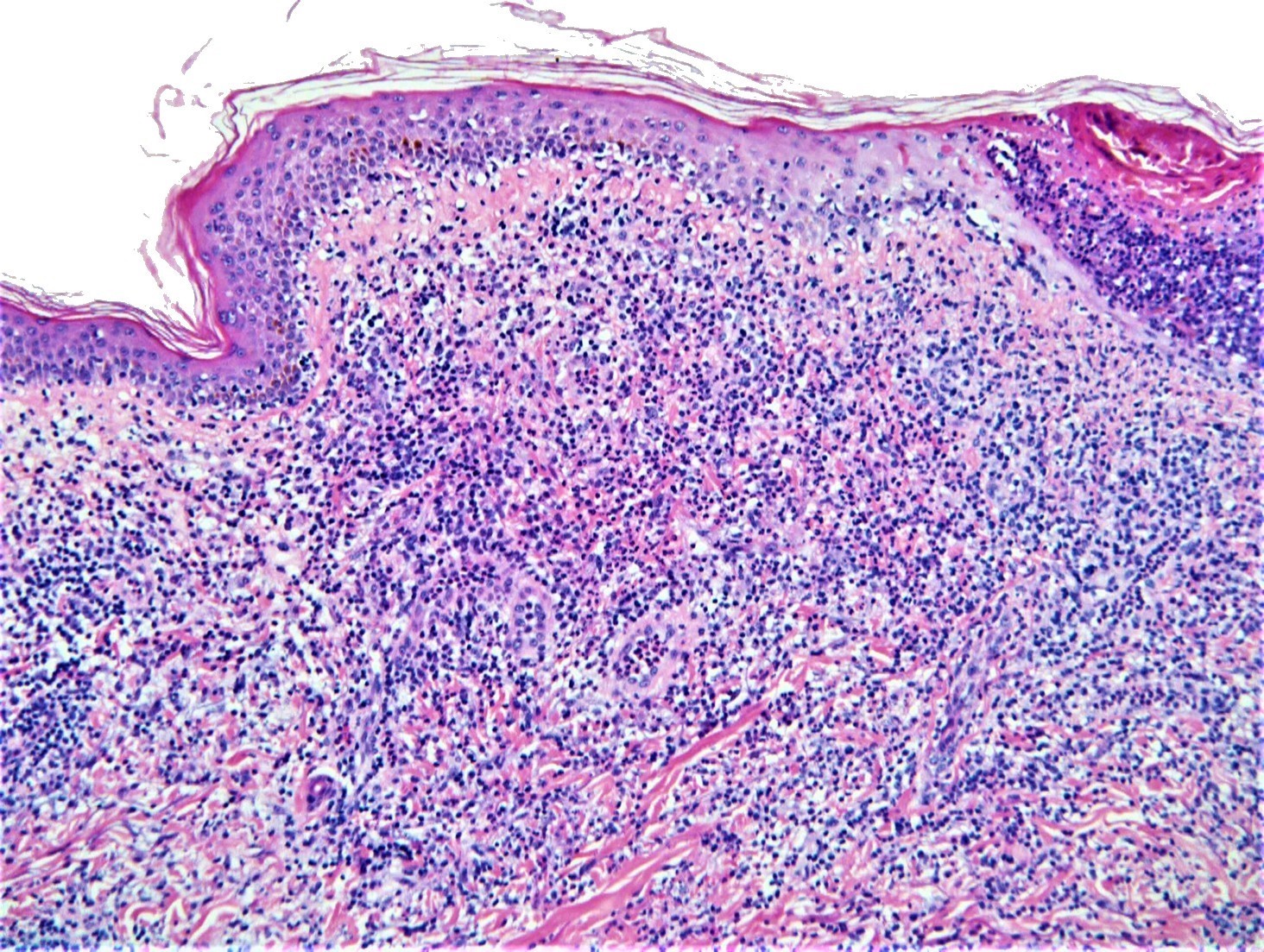
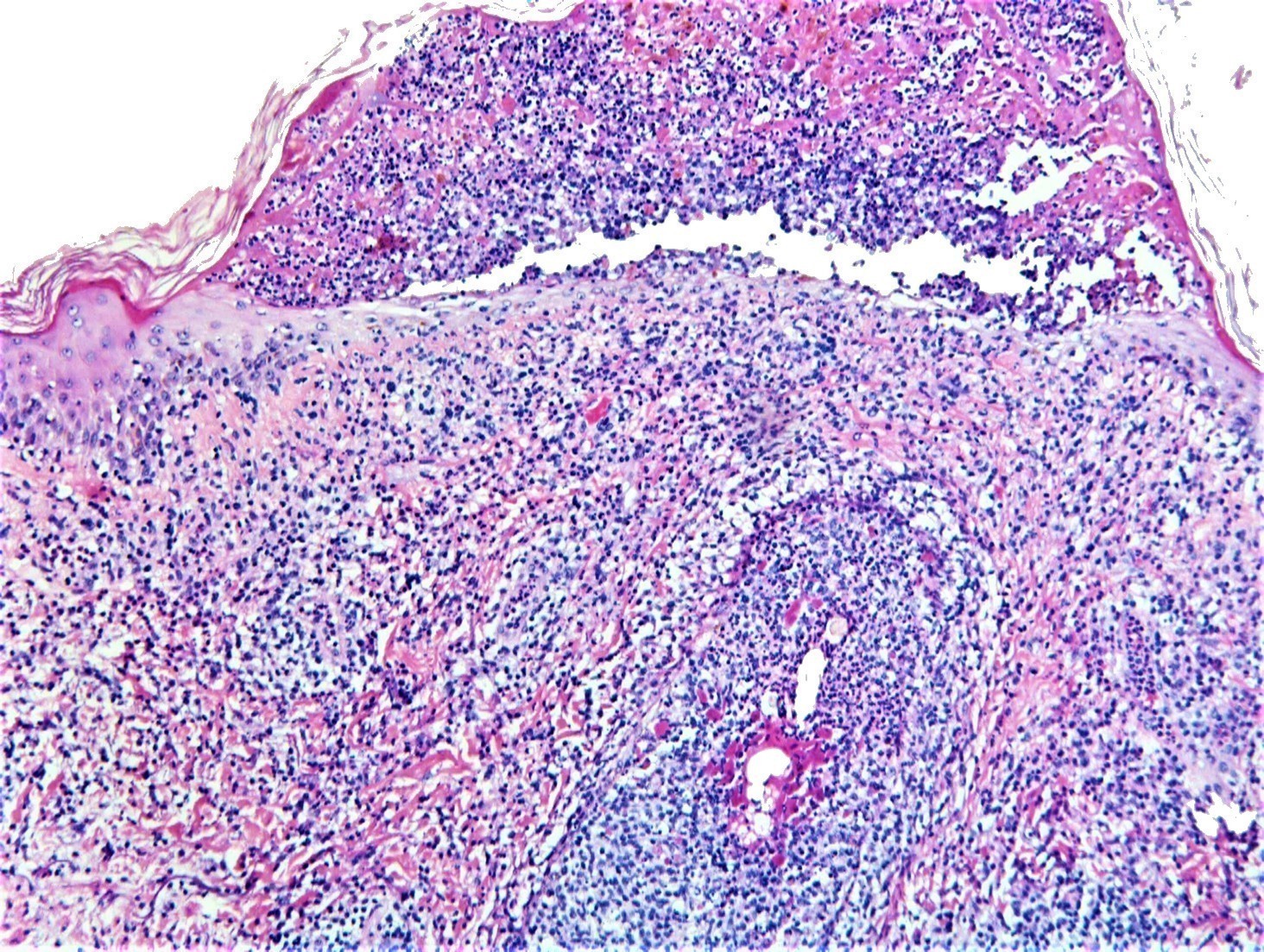
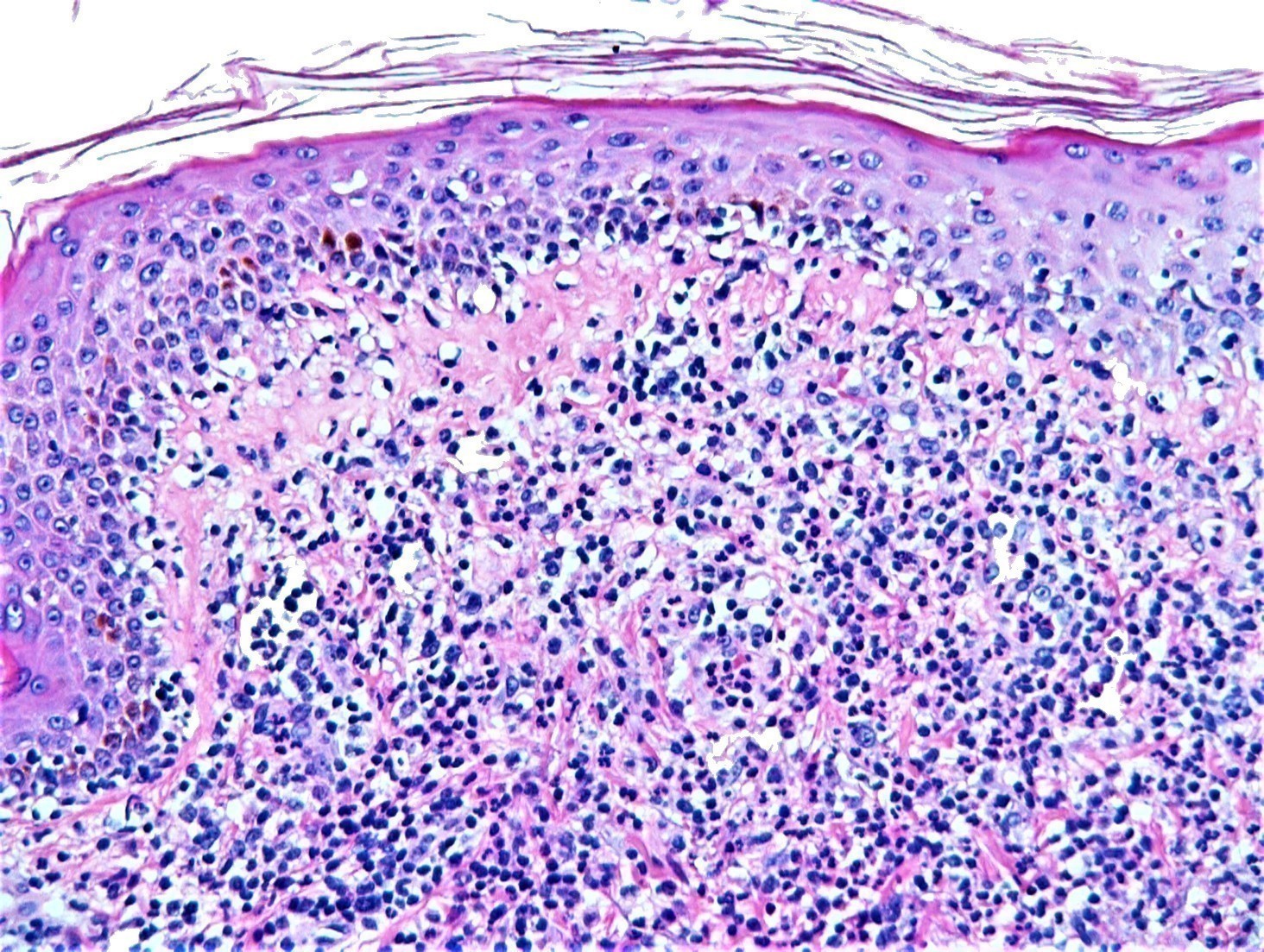
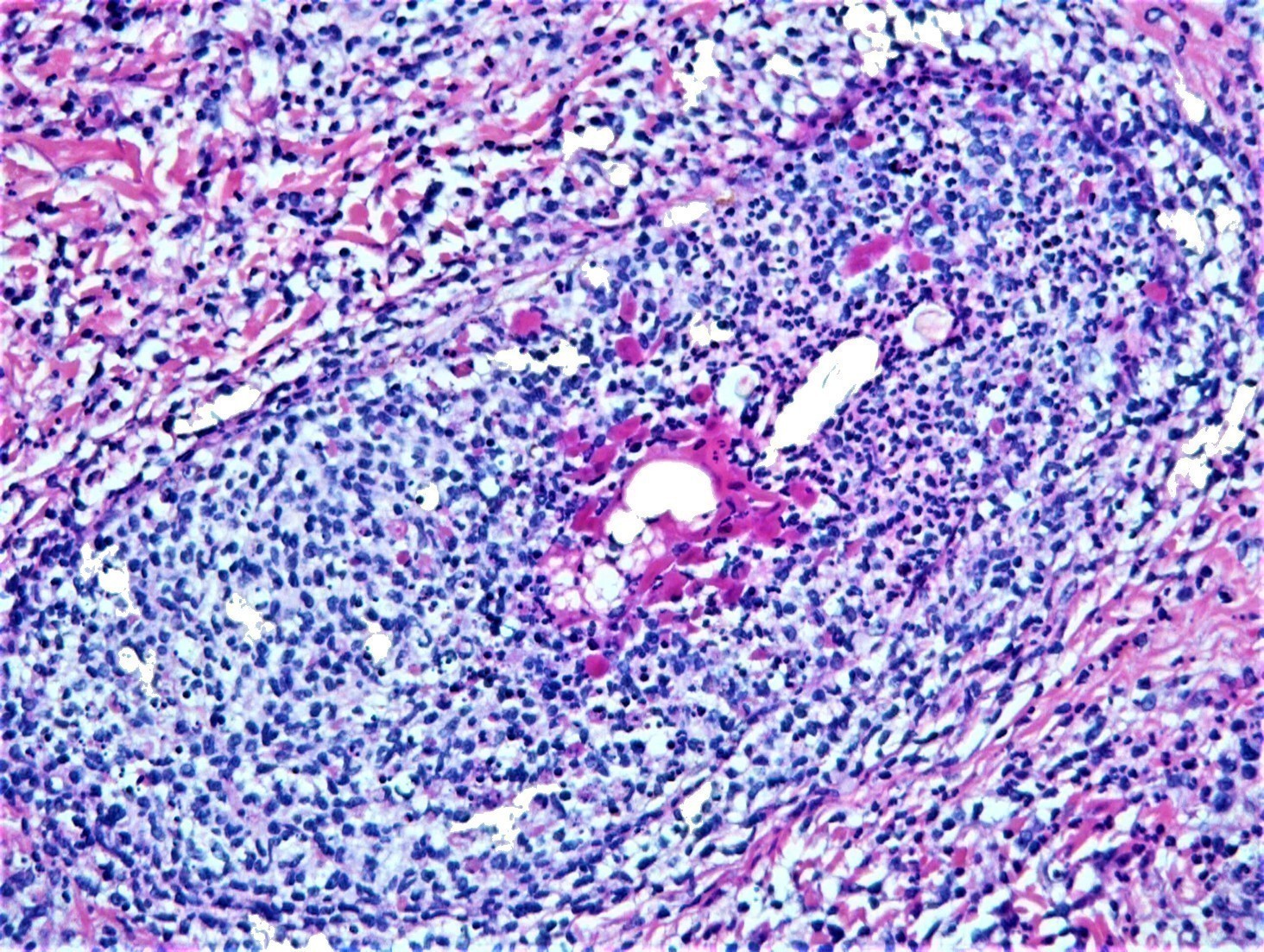
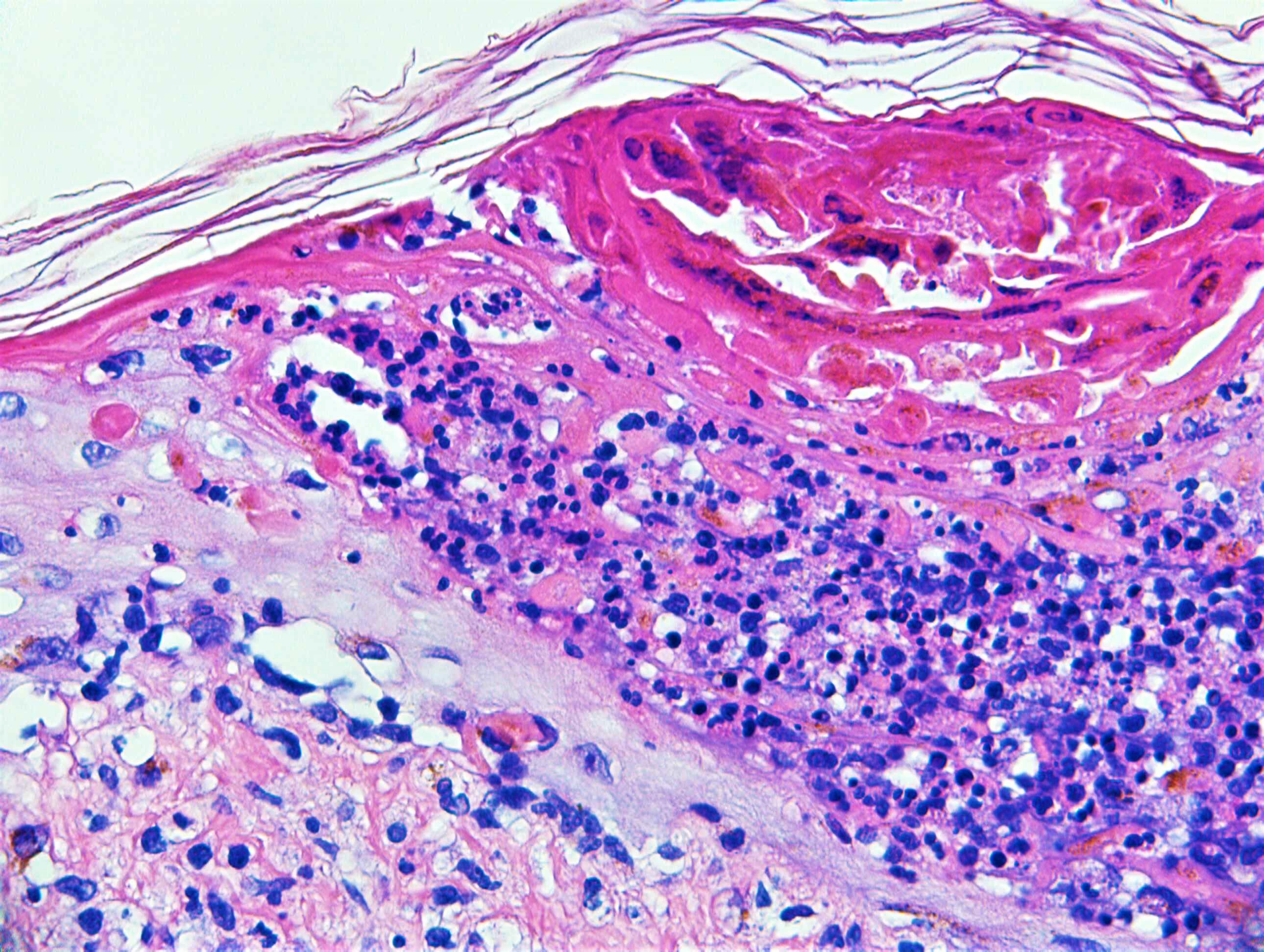
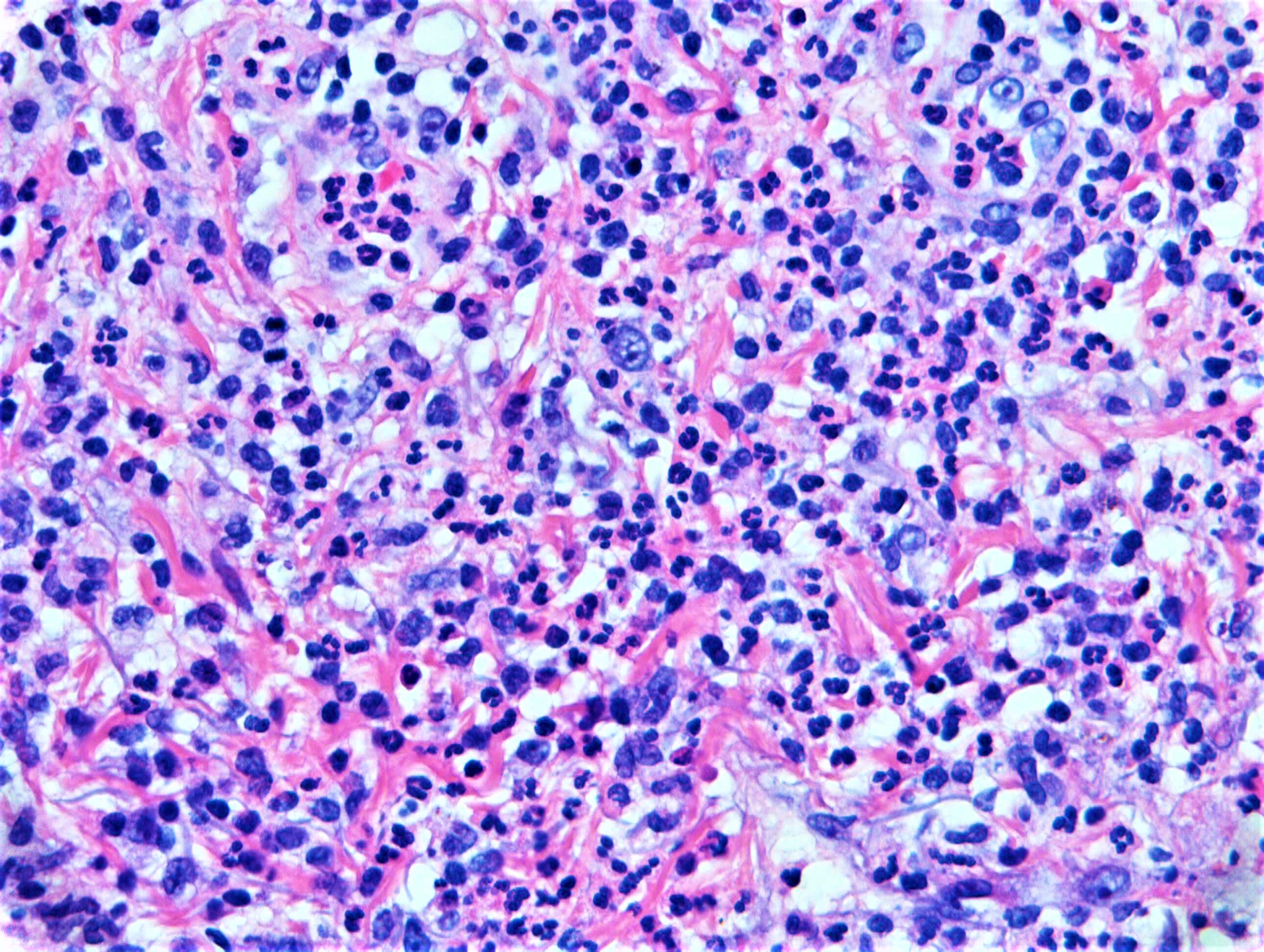
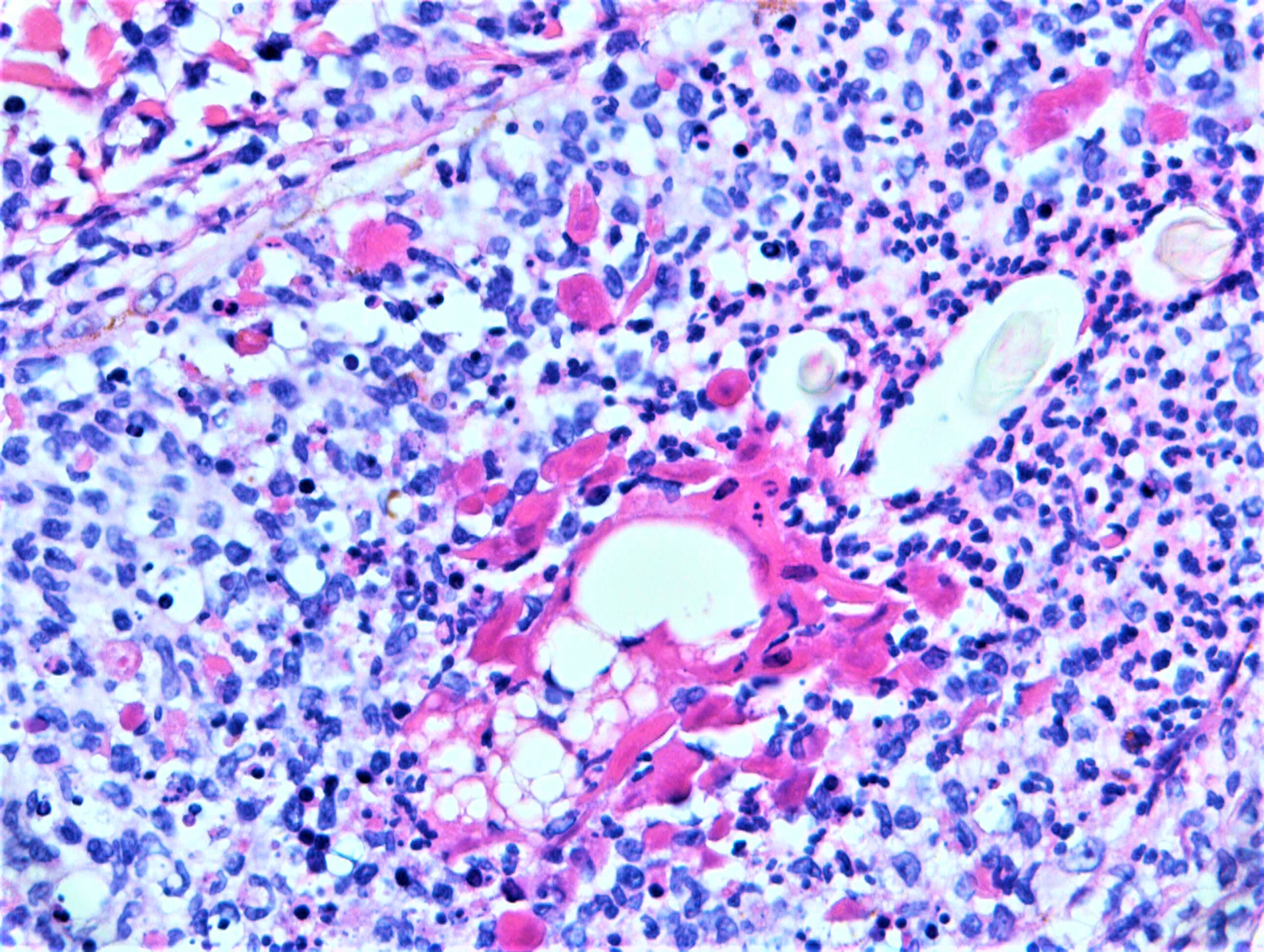
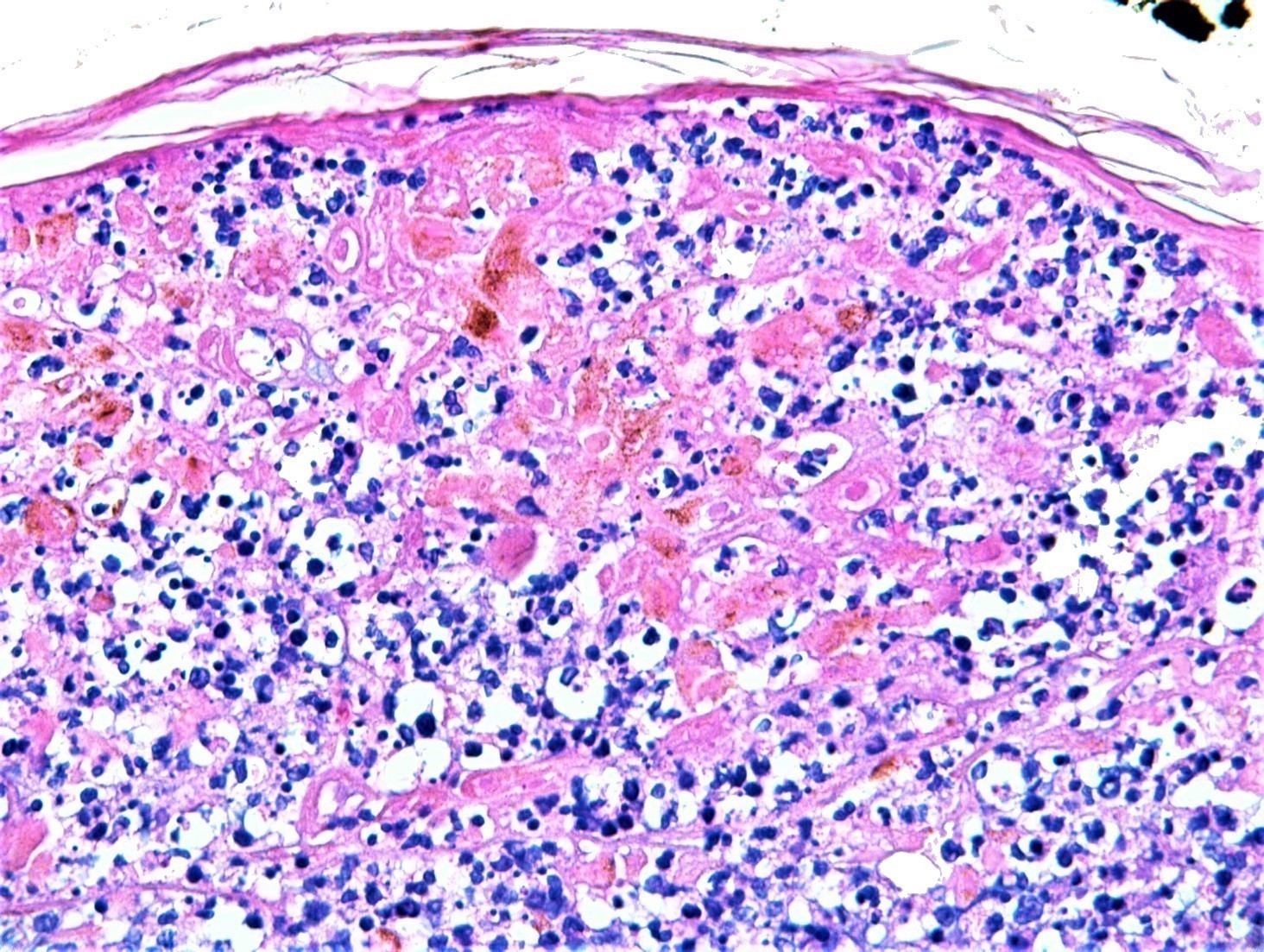
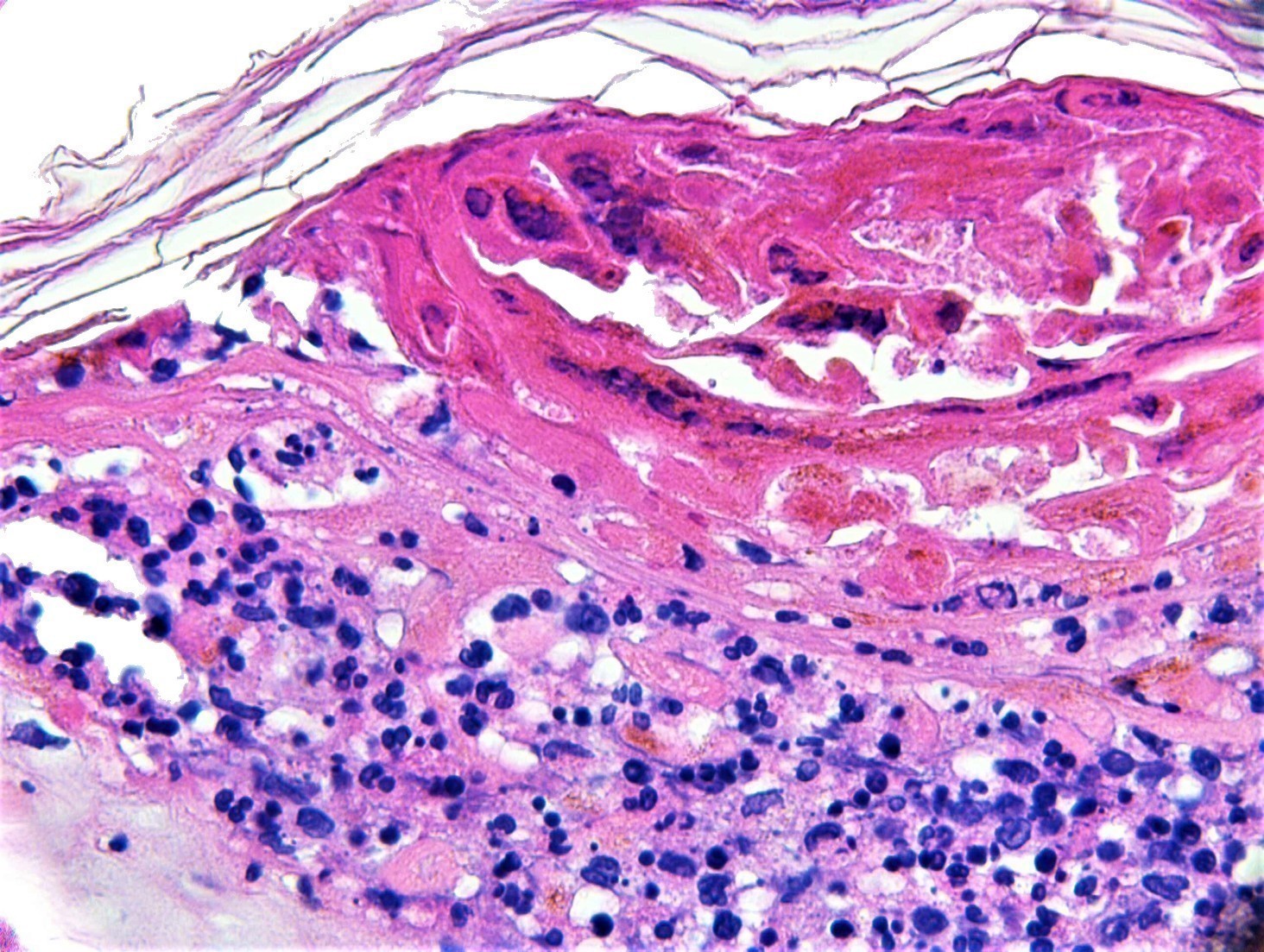
F65. Pervious history of low grade NHL with high grade transformation. Plaque on cheek.

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.