Case Number : Case 1202 - 30th January Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
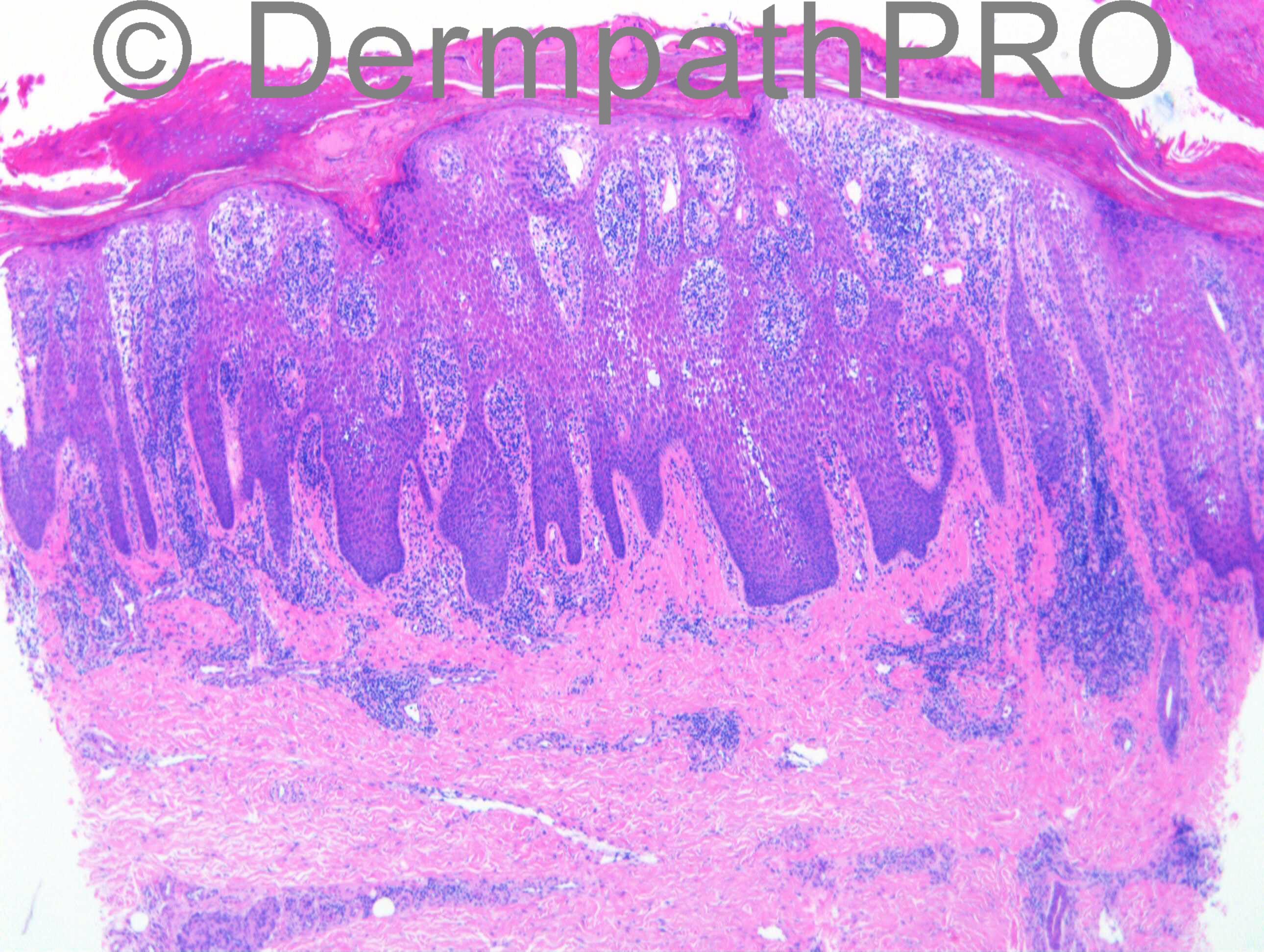
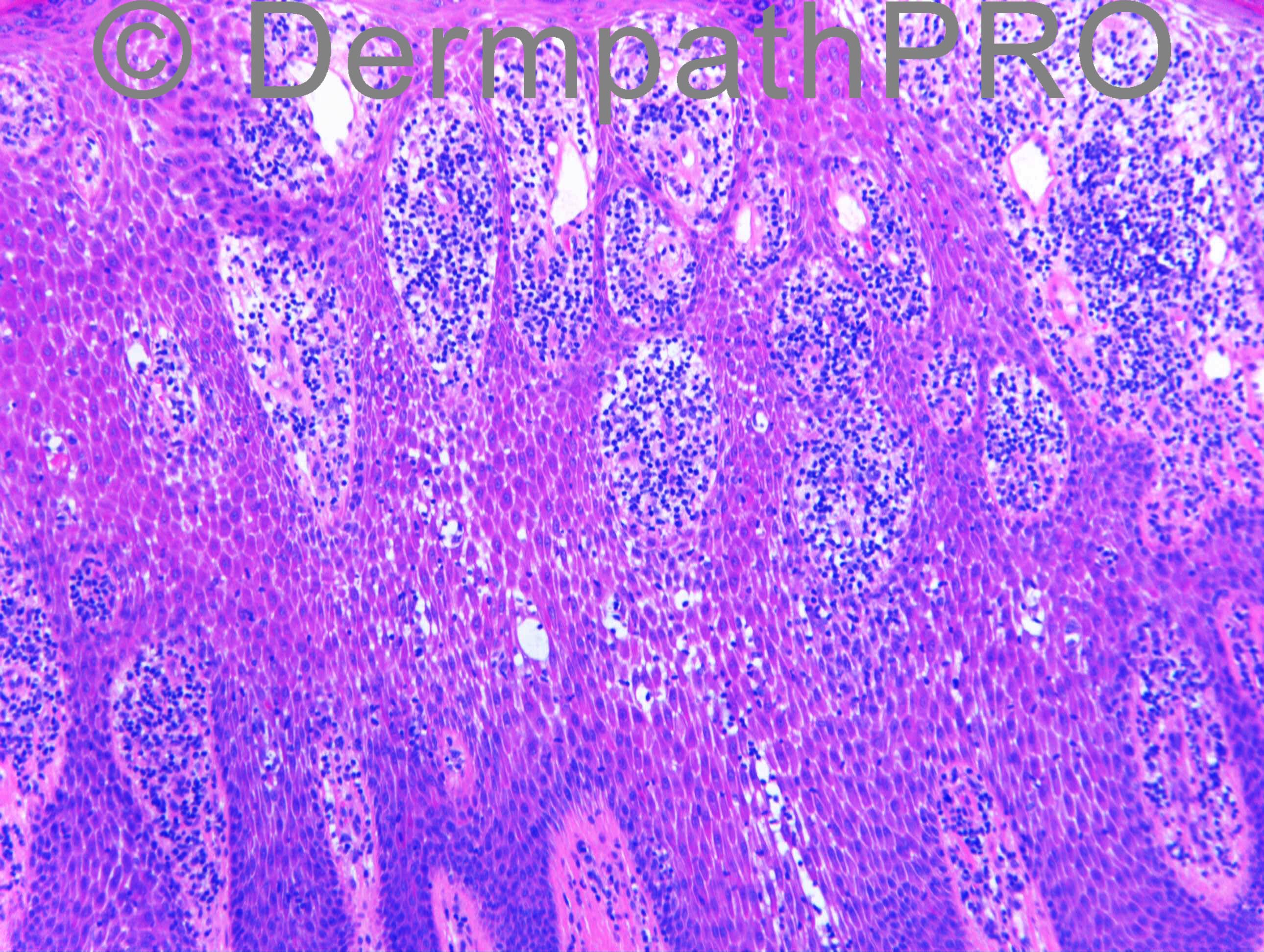
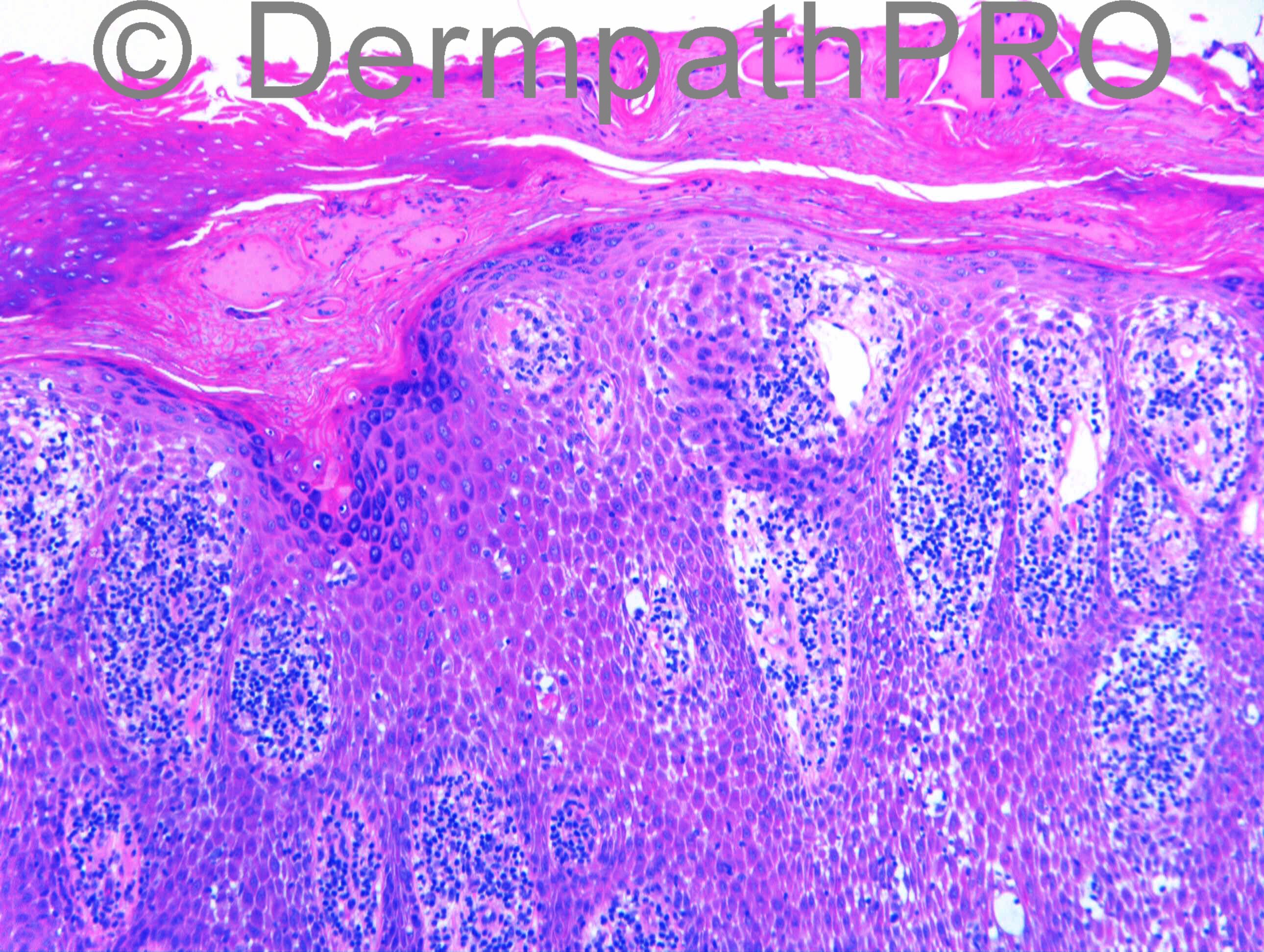
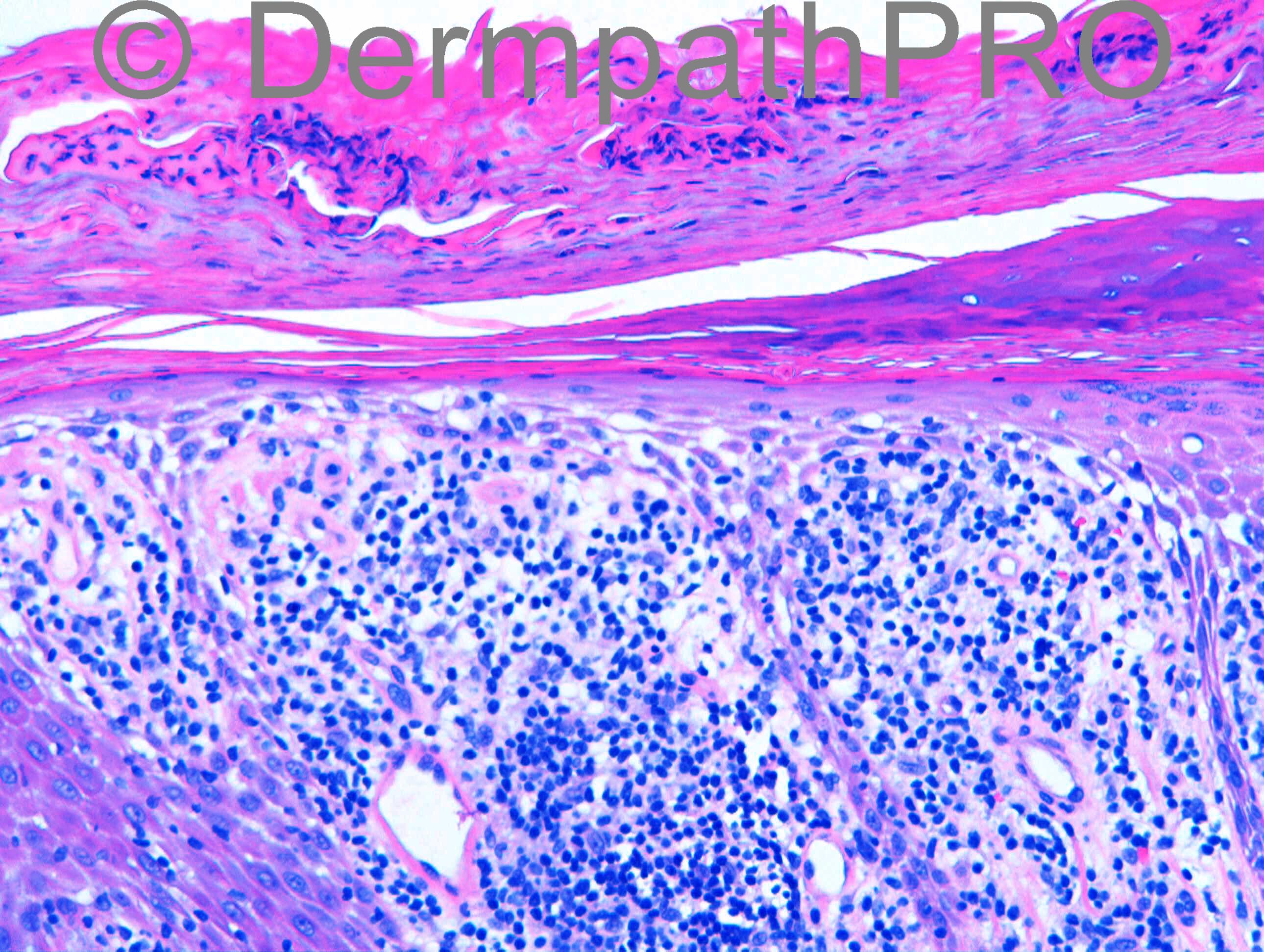
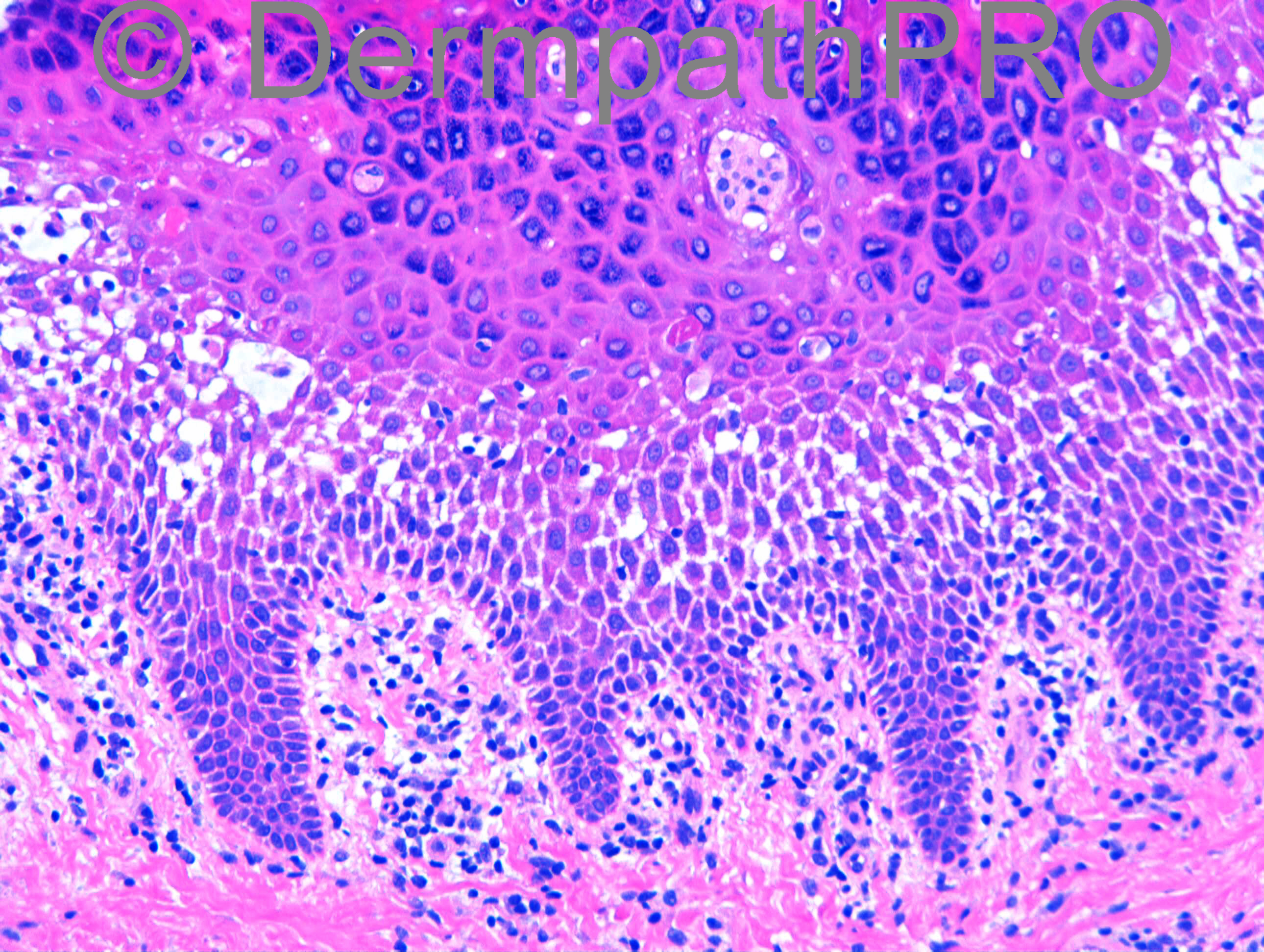
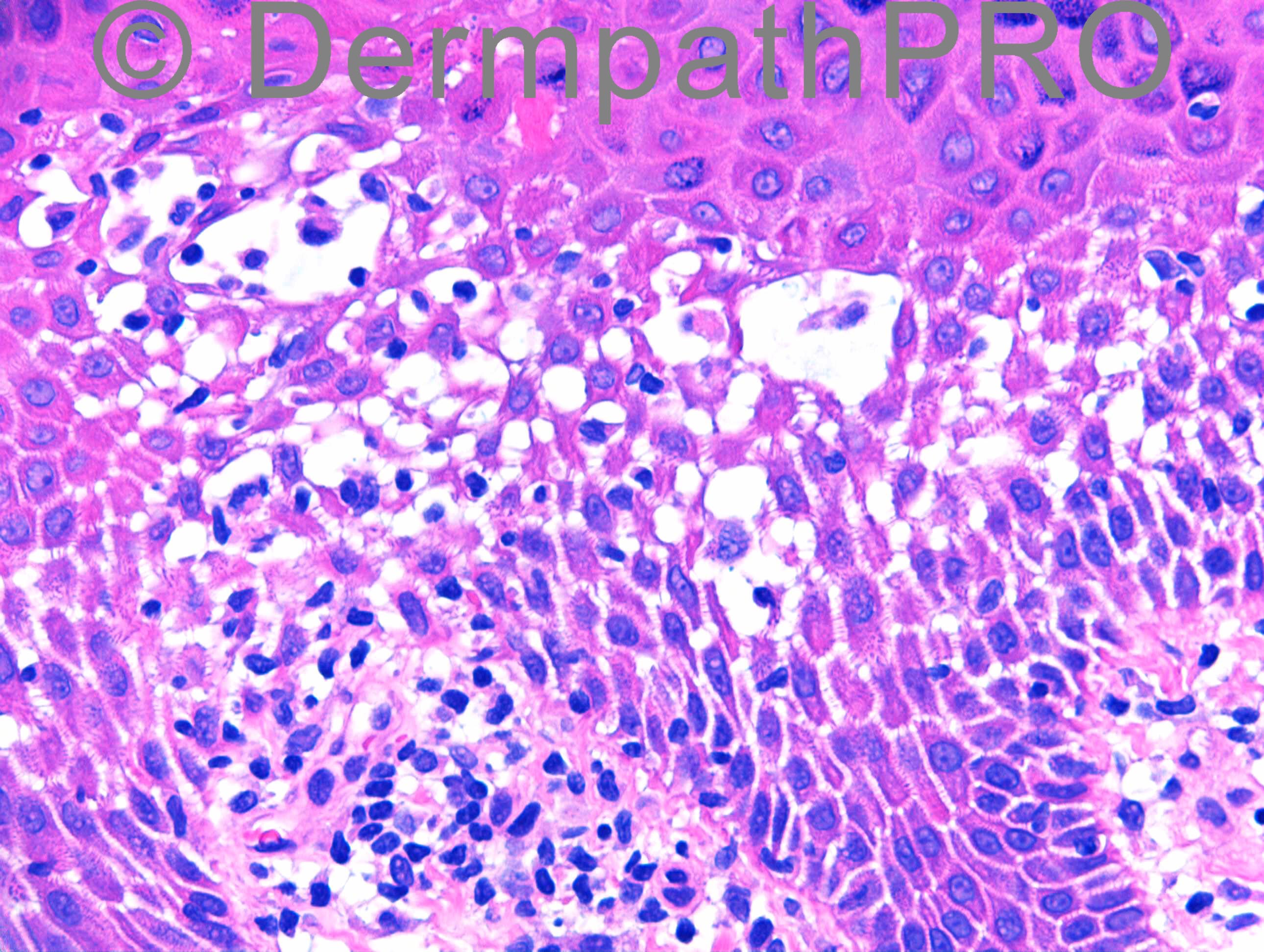
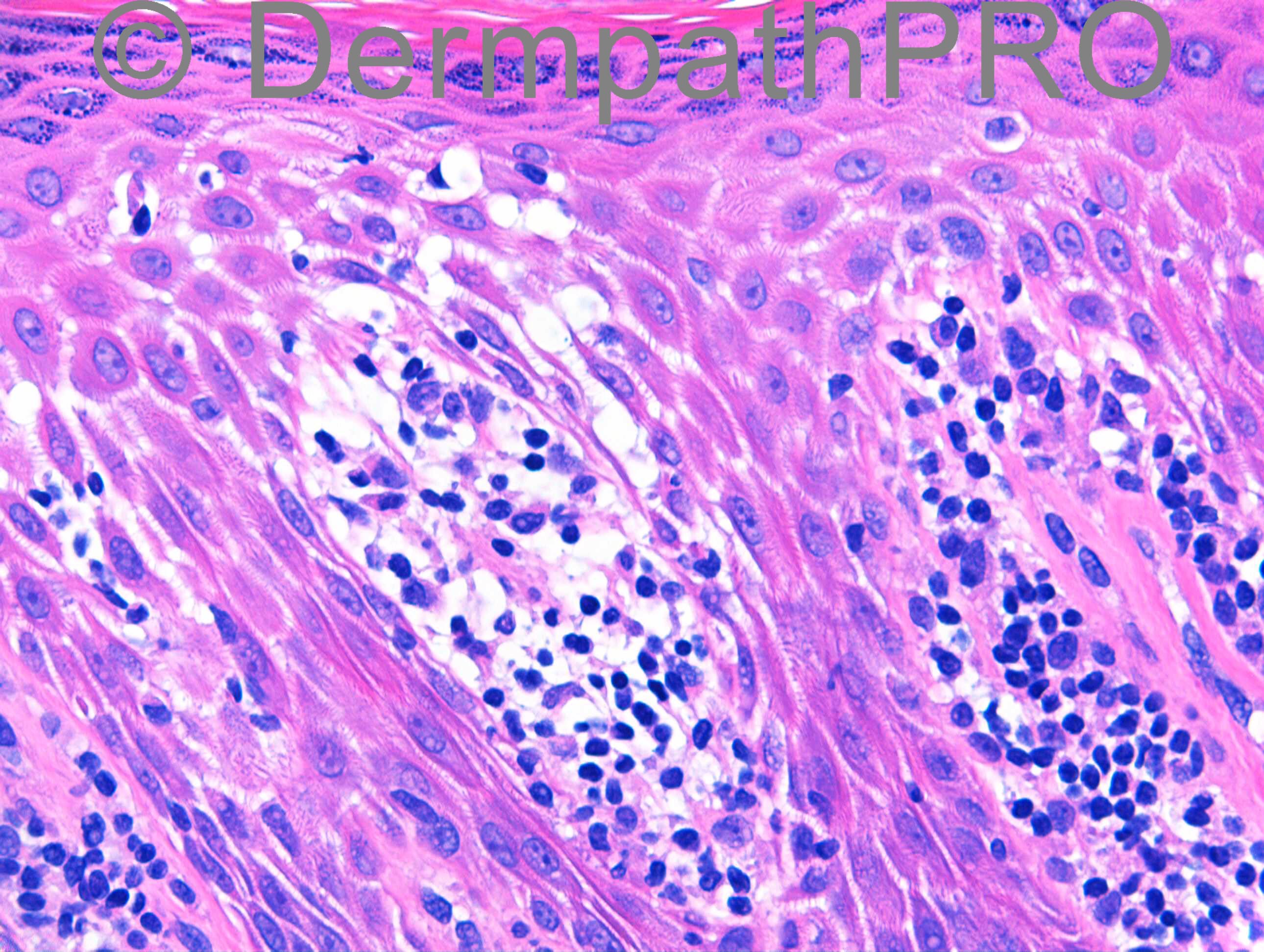
M31. Left palm biopsy. 3y well demarcated hyperkeratotic plaques on left palm and erythematous papules on left wrist and right shin. No nail psoriasis. DD: Psoriasis, eczema, CTCL
Case posted by Dr Richard Carr
Case posted by Dr Richard Carr


Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.